Skip to
A food-drug interaction is when a particular food or drink affects the way in which a certain medication works. The risks of food-drug interactions include preventing the proper working of a medication, causing unwanted side effects, and changing the way the body uses ingested food or beverages while on the medication.
Medications can also work differently if they are taken on an empty stomach. For instance, they may work faster or slower, more or less effectively, or cause digestive problems.
It is important to discuss potential interactions between existing and new medications to prevent or recognize any side effects. This caution also extends to drug-food interactions.
What are anticoagulants?
Anticoagulants, commonly called blood thinners, are a group of medications that impede the blood clotting process. They are prescribed to avoid the development of harmful blood clots. Anticoagulants are commonly used in the treatment of diseases in which there is an increased risk of blood clot formation. These include deep vein thrombosis, factor V Leiden, myocardial infarction, and polycythemia vera, among many others.
When anticoagulants are prescribed, a prothrombin time (PT) test is used to evaluate its effectiveness. This test looks at how quickly the blood clots.
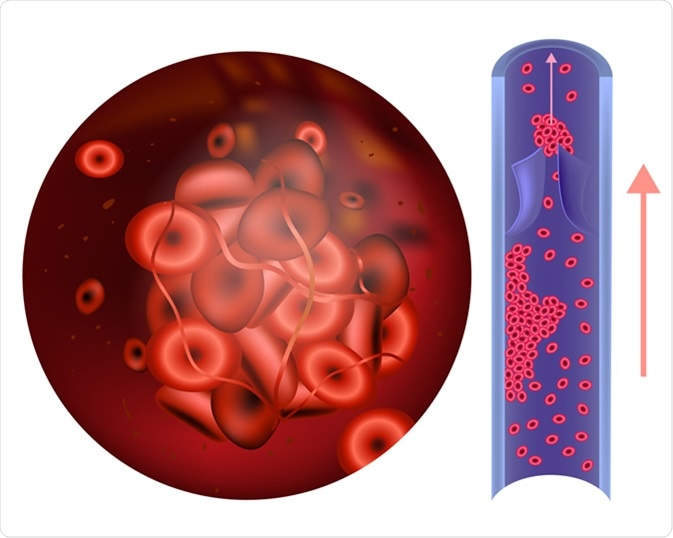
Prothrombin thrombophilia. (sometimes hypercoagulability or a prothrombotic state) Image Credit: Sakurra / Shutterstock
Results from the PT test are expressed as a ratio called the international normalized ratio (INR).
An INR value of 1.1 or below is considered normal in healthy patients, with lower values indicating faster clotting, while higher values show slower clotting rate. INR values of between 2.0 and 3.0 are considered effective therapeutic values while on anticoagulant therapy.
Vitamin K antagonists
Vitamin K antagonists (VKAs) are the most commonly prescribed oral anticoagulants worldwide. They are used to treat conditions such as embolic ischemic stroke, deep vein thrombosis, and pulmonary embolism. Interactions which affect the efficacy of VKAs may result in bleeding from over-anticoagulation, or thrombosis due to under-anticoagulation.

A spoon with tablets of warfarin sodium. Warfarin is a Vitamin K antagonist which is used for preventing the blood from clotting. Image Credit: Dajra / Shutterstock
Direct oral anticoagulants (DOACs)
Direct oral anticoagulants (DOACs) are expected to replace VKAs because of their increased safety margin. However, interactions with food, drinks, herbs, and other medications may still occur.
Anticoagulants and vitamin K interactions
Vitamin K is a necessary element in the blood clotting process. Adults need approximately 1 microgram/kg body weight of vitamin K a day. If excess vitamin K is taken, it is stored for future use in the liver. As such, daily intake or extra supplementation with vitamin K is typically unnecessary to keep body stores at healthy levels.
Vitamin K is found in the following foods:
- Liver meat
- Broccoli
- Brussels sprouts
- Cabbage
- Cheese
- Collard greens
- Kale
- Lentils
- Flaxseed
- Lettuce
- Spinach
- Soybean oil
- Turnip greens
- Camomile
- Green tea
Flaxseed may inhibit the proper absorption of anticoagulants.
Soybean oil or soybean milk, as well as liver, has high vitamin K content, which may interfere with the action of VKAs.
Cranberry products are not significant unless taken in high amounts, as for urinary infections.
Green tea in high amounts could reduce PT-INR values.
Camomile in large quantities, a herbal treatment that is used to treat anxiety, catarrh and gastric problems, has also been implicated in a case of severe bleeding in a 70-year-old woman.
Mango and St. John’s wort are also clinically relevant inhibitors of VKAs.
Anticoagulants and alcohol interactions
Alcohol interacts with a large number of medications.
It is important to note that alcohol also has some anticoagulant action and can protect adults from blood clots, although it is not recommended as a preventative measure for this purpose.
The liver is responsible for breaking down alcohol and some medications, and this may cause a slower than normal metabolism of the anticoagulant, increasing the drug concentration in the blood, and hence the risk of bleeding.
When taken with anticoagulants, binge-drinking alcohol can increase INR values. On the other hand, chronic alcohol consumption reduces the INR. It is recommended that patients on anticoagulants drink two or fewer alcoholic drinks per day.
Anticoagulants and herbal supplement and vitamin interactions
A variety of herbs and vitamins may interact with anticoagulants.
Cranberry juice and other cranberry products can alter the effects of anticoagulants. Large amounts of garlic, ginger, glucosamine (an amino sugar), ginseng, and ginkgo should be avoided while on anticoagulant medications as they may increase the risk of bleeding.
The following supplements are theoretically capable of inhibiting VKAs, but their clinical effect is insignificant:
- Feverfew
- Fish oil
- Omega-3 fatty acids
- Garlic
- Ginger
- Ginkgo
- Turmeric
- Curcumin
Studies have shown that there is a 58% higher likelihood of achieving PT-INR values in the optimal therapeutic range of 2.0 to 3.0 if patients on VKA medication avoid herbal supplements or take them three or fewer times a week.
Fish oils may increase a patient’s INR level, and as such INR levels should be checked if a patient on anticoagulants begins to take significantly higher amounts of fish oil.
Summary
It is generally advised that patients taking anticoagulants keep to a balanced and consistent diet balanced throughout their treatment course to avoid fluctuations in treatment efficacy. It is advised that vitamin K intake through diet (chiefly through liver meats, high amounts of green leafy vegetables, and cranberry juice) also be closely monitored in such patients for the same reason.
Further Reading