The coronavirus disease 2019 (COVID-19) pandemic was caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This novel coronavirus causes mostly asymptomatic or mild infection, but in a sizable minority, it triggers a hyper-inflammatory response that leads to severe or life-threatening disease.
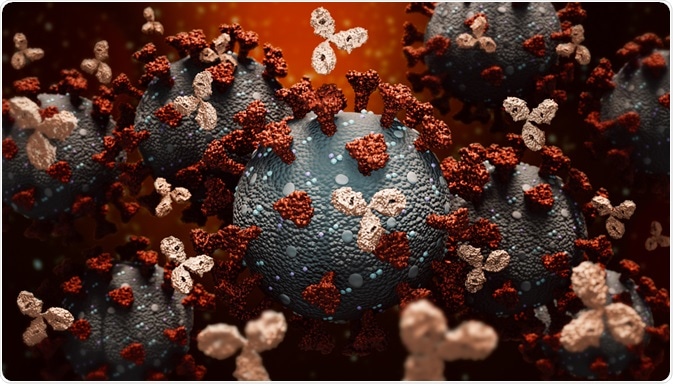
Image Credit: MattLphotography/Shutterstock.com
Background
The viral genome is composed of single-stranded ribonucleic acid (RNA) that encodes four structural proteins and a number of nonstructural and accessory proteins. The structural proteins are the spike (S), envelope (E), membrane (M), and nucleocapsid (N) proteins.
The spike protein mediates viral attachment to the host cell receptor, the angiotensin-converting enzyme 2 (ACE2), and entry via viral-cell membrane fusion or endocytosis. This occurs at the receptor-binding domain (RBD), where the S1 domain of the spike protein engages the receptor. This binding leads to a massive conformational change in S2 to the post-fusion state of the protein.
Monoclonal antibodies (mAbs) are proteins formed against a foreign antigen. These are created by incubating immune cells with a specific viral protein to produce one specific antibody. The white cell is then cloned so that it can be a cell factory churning out antibodies against the target pathogen.
Monoclonal antibody EUA criteria
Monoclonal antibodies (mAbs) directed against the spike protein have been found to be clinically useful in the therapy of COVID-19. At present three mAbs have received Emergency Use Authorizations (EUAs) from the Food and Drug Administration (FDA).
It is important to remember that EUA is not tantamount to approval by the FDA. The COVID-19 Treatment Guidelines Panel advises using one of the following mAb cocktails for the treatment of mild-to-moderate COVID-19 in patients who are not sick enough to require hospitalization but have multiple risk factors for severe disease and hospital admission.
The EUA criteria have been broadened to include patients with a body mass index (BMI) of 25 or above, pregnant patients, and racial/ethnic factors. Also, patients with medical high-risk conditions such as sickle cell anemia, asthma cardiovascular disease, and disorders of neurological development are now eligible at any age above 12 years.
However, all such conditions have not been tested in trials, so the strength of the evidence for their inclusion in treatment criteria is low. In fact, the details regarding the methodology and designs of these trials have not yet been reviewed, and further changes may occur once this is completed.
Available antibodies
The mAbs in question are:
1) A cocktail of bamlanivimab plus etesevimab, neutralizing mAbs that recognize different epitopes that overlap each other in the RBD. These are less effective at neutralizing the newer Beta and Gamma variants of concern of the virus. Thus, their use is indicated where the prevalence of such variants is low.
2) A cocktail of casirivimab plus imdevimab, recombinant human mAbs that engage distinct non-overlapping epitopes of the RBD. This is given intravenously, but if this is non-feasible or would delay treatment, the dose is split into four subcutaneous doses given at one time. This condition is due to the limited safety and efficacy data on this route.
3) Sotrovimab, first identified in a SARS-CoV patient who recovered from the infection but found to engage an epitope in the SARS-CoV-2 RBD that is common to both viruses. Here, the relative risk reduction was 85%, with an absolute risk reduction of 6%.
Current recommendations
Recommendations include initiation of treatment as early as possible after a diagnosis of SARS-CoV-2 infection and not more than 10 days of the onset of symptoms. Secondly, patients with mild-to-moderate COVID-19 should be treated with mAbs if the above criteria are fulfilled, even if hospitalized, as long as the hospitalization is not related to the diagnosis of COVID-19.
Thirdly, these mAbs are not useful for the treatment of patients with severe COVID-19, such as those hospitalized with this condition, those who need to be on oxygen, or those already on oxygen who require increased flow rates due to the superimposed oxygen flow rate.
They may, rarely, be used if the patient fails to seroconvert or is immunocompromised and unlikely to respond robustly to the immune challenge. There is no evidence for their use in the latter setting so far.
Secondly, mAbs may be useful in preventing the spread of SARS-CoV-2 infection between household members, for instance, or within a long-term care facility. The FDA has extended EUA for the second cocktail for use in preventing the infection in exposed individuals who have an increased risk of infection as well as of disease progression.
Why these recommendations?
The basis of this recommendation is the finding that mAbs reduced the risk of hospitalization and death when used in such patients, from randomized controlled trials. However, since these trials were held at a time when there were few variants of concern, further research is required to establish their utility in treating infections with these variants which may show partial resistance.
The Alpha variant remains as susceptible as the wild-type virus. The Beta and Gamma variants are much less susceptible to casirivimab, bamlanivimab, and etesevimab, but the casirivimab plus imdevimab combination remains powerfully neutralizing, as does sotrovimab. Both these variants contain the E484K mutation as well as K417N/T, respectively.
The Delta variant contains the L452R mutation, and is somewhat less susceptible to the bamlanivimab-etesevimab cocktail in vitro, remaining vulnerable to neutralization by sotrovimab and the casirivimab plus imdevimab combination.
The Epsilon and Iota variants show the same pattern, though the E484K mutation in the latter is associated with partial resistance to casirivimab in vitro.
With cocktail 1, the risk of hospitalization or death due to COVID-19 was 1%, vs. 3.2% in the placebo. This translates to a 70% reduction in risk relative to the placebo group, but in absolute terms, the risk is low in both groups.
In the RECOVERY study, patients hospitalized with COVID-19 who did not seroconvert benefited significantly from the combination of casirivimab plus imdevimab, with an absolute reduction of 6% in the mortality (24% vs. 30% in the mAb and standard of care groups, respectively).
Caveats to this include the fact that this study used a higher dose of mAbs than used under the current EUA, which does not allow for the routine use of these drugs in hospitalized patients with COVID-19; also, seroconversion is not routinely assessed at present due to the lack of rapid testing resources.
The use of mAbs in children with COVID-19 who are not hospitalized but have risk factors for progression of the disease is not backed by evidence, but either cocktail 1 or 2 may be used on a case-by-case basis if the EUA criteria are fulfilled.
Vaccination after mAb treatment
The potential for interference with the immune response by the passively administered mAbs has led to the advice to delay COVID-19 vaccination for at least 90 days from the date of receiving the mAbs.
Adverse effects
The adverse events reported in individuals who have received mAbs to SARS-CoV-2 include hypersensitivity reactions, including anaphylaxis and reactions to the infusion. Itching, dizziness, and rashes, as well as gastrointestinal symptoms like nausea and diarrhea, may also occur.
No drugs are thought likely to interfere with these mAbs. In pregnant women, particularly if they have risk factors for COVID-19 progression, mAbs should be used. The rationale for this guideline is the fact that immunoglobulin G (IgG) antibodies have been used in pregnancy in other settings.
Future trials should incorporate pregnant women into testing cohorts, as well.
References:
Further Reading